


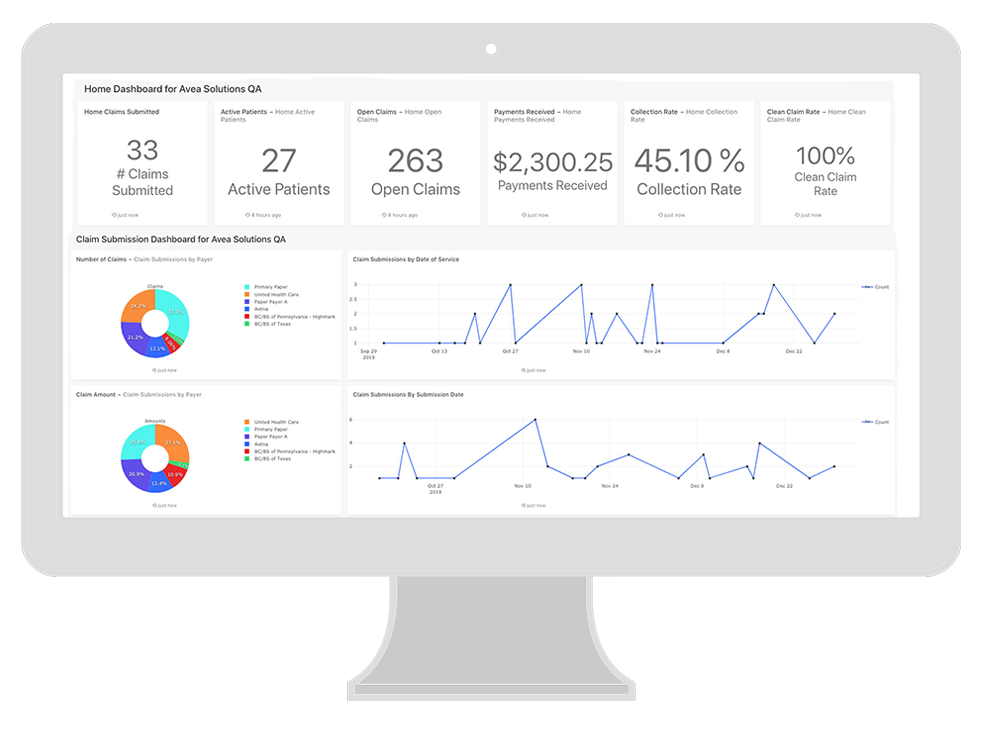
CLICK TO VIEW LARGER
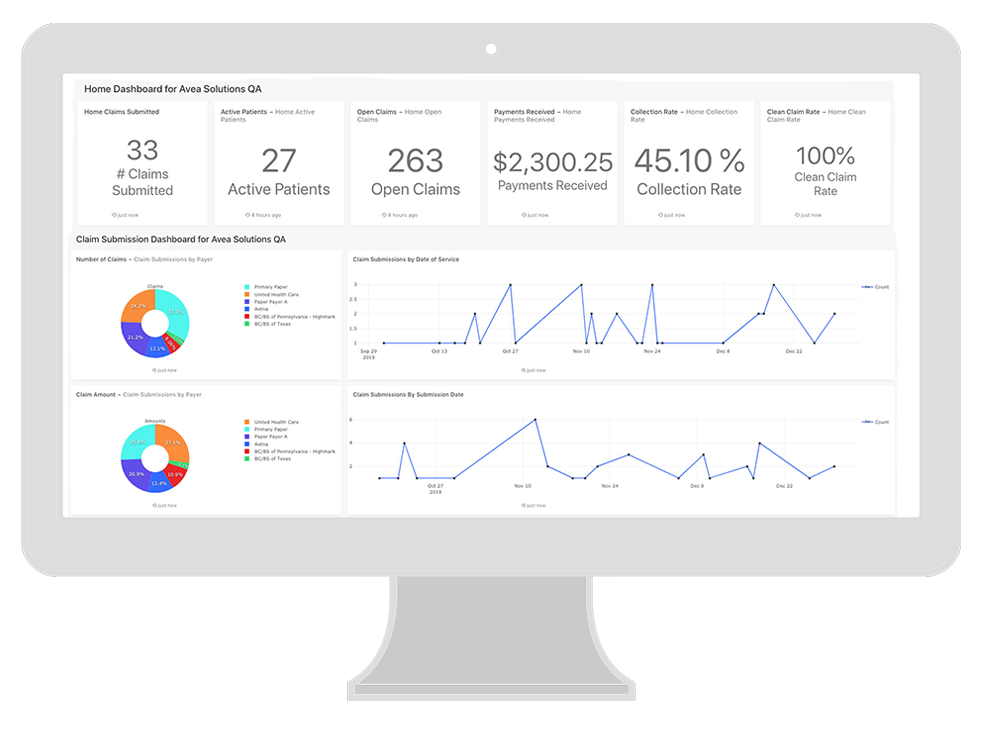
CLICK TO ENLARGE


We are proud to do our part in supporting addiction and substance use disorder treatment facilities for the life saving work you do. Our mission is to help you get paid fully and quickly for the services you provide by bringing you revenue cycle management software that gives you full visibility into your financial operations, supports your teams with the tools they need to bill correctly and collect efficiently, and that offers you a sense of control over your business so you can spend more time with your patients – and less managing your claims and chasing payments.
9450 SW Gemini Dr
Suite 22100
Beaverton, OR 97008-7105